
As the weather warms up, it is more important than ever to make sure you and your furry friends are protected against ticks. Tick paralysis is a serious and potentially fatal condition requiring urgent attention.
Ticks feed on blood of humans and animals. They can cause severe allergic reactions and transmit diseases to their hosts. Infection can result from the bite of an infected tick or from exposure to the faeces of infected hosts.
Killing a tick safely and as soon as possible after you notice it can help prevent tick-related illnesses.
1. What are Ticks?

Ticks are parasites that feed on animal and human blood. They attach to the skin by piercing their mouthparts onto it. They attach themselves to soft areas such as armpits groin and scalp.
They are found in moist bushland parks and gardens especially on the Eastern coastline of Australia There are around 70 species found in Australia with 16 species able to feed on humans.
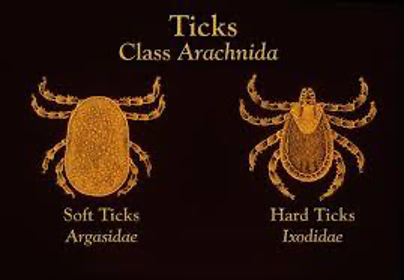
There are two main groups: –
- Hard ticks have a hard, flat body and elongated mouthparts with rows of pointing teeth. These are the main species that bite humans.
- Soft ticks have a wrinkles leathery body, they rarely encounter humans.
They are not very mobile but rely on passing animals to both feed on and transport them. Ticks are known to inject toxins that cause local irritation which can either be mild or severe. Most tick bites cause little or no symptoms, but some give the disease, tick paralysis and can pose a serious health threat.
2. What are the common tick-borne diseases?

Tick-bourne diseases are illnesses from infections that can be transmitted to both humans and other animals via tick bites which cause a serious health threat.

- Australian Tick Typhus or “Spotted Fever” which includes Queensland Tick Typhus occurring along the coastal strip of Eastern Australia from North Queensland to Victoria.
- Flinders Island Spotted Fever occurring in Victoria, Tasmania, and Flinders Island in Bass Strait.
- Lyme disease has not yet been proven to be linked to ticks in Australia. There are concerns that other serious illnesses, such as a Lyme disease-like syndrome, may be caused by exposure to Australian ticks, however there is no evidence yet this is the case.
What happens when a Paralysis Ticks BITES?
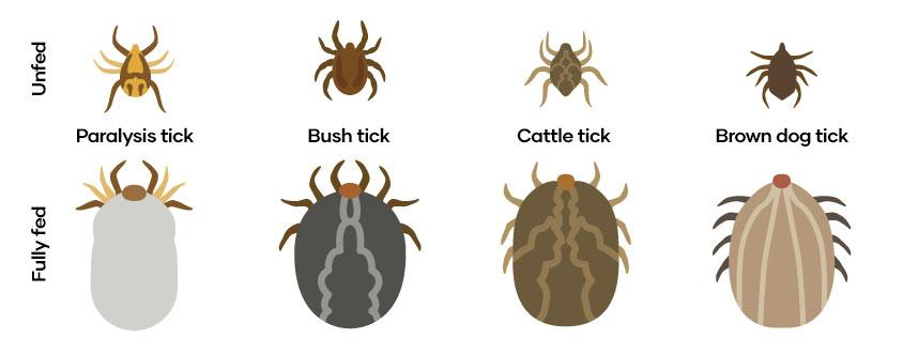
Over 90% of tick bites and tick bourne illness in Eastern Australia are due to the Paralysis Tick. It is commonly referred to as the grass tick, seed tick or bush tick, depending on its stage of development.
The tick attaches itself by piercing its sharp mouthparts into skin. It then injects its saliva containing an anticoagulant, which is a substance that stops blood from forming clots. In the case of the Paralysis Tick, the saliva can be highly toxic to some animals and potentially, humans.

Once the tick is attached it becomes deeply and securely embedded in the skin. When an adult tick feeds on blood, it increases greatly in size. The area of attachment on the skin becomes red and a raised thickening or ‘crater’ forms. A crater is also evidence of a previous tick attachment.
4. What do the different stages of ticks look like?
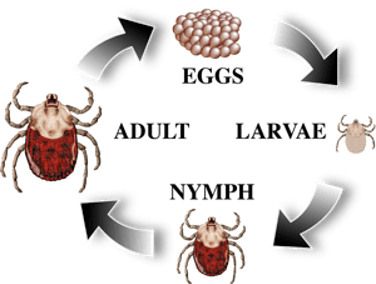
There are four stages in the life cycle of a tick, the egg, larvae, nymph, and adult. The adult tick is around 4-5mm in length. The Paralysis Tick needs to feed on blood to develop through its lifecycle from larvae to nymph and to adult. The adult female takes blood to obtain protein for the laying of the eggs.
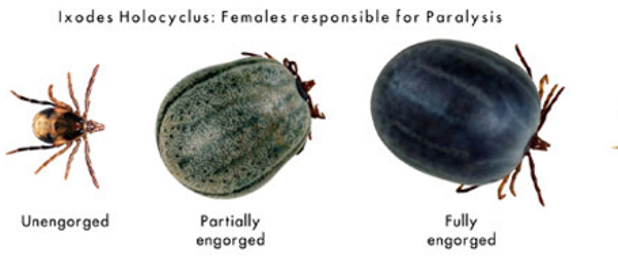
The paralysis tick can look different depending on whether they are engorged with blood or not. Once they are engorged with blood, they take on a different appearance greatly increasing in size and changing to a grey – blue colour, up to around 1cm in length.
Paralysis ticks are dangerous parasites. They drain the blood and secrete a toxin which affects the animal’s nervous system causing serious illness and is potentially fatal.
5. What are the Symptoms of Tick Bites?

Most tick bites do not cause any symptoms, but it is important to seek medical attention if any of the symptoms develop. The tick paralysis symptoms may intensify as the tick engorges on more of the host’s blood or even after the tick has been removed. Tick paralysis and severe allergic reactions can pose a serious health threat
Tick related illnesses:
- Allergic Reactions. Local skin irritation causing swelling and redness lasting for several days. Rash (spotted or circular)
- Life-threatening anaphylactic reactions (which can cause localised “burning”, widespread itching and swelling, throat swelling, trouble breathing and collapse)
- Flu like symptoms, including fever, breathing difficulties with a swelling of the throat, tenderness of lymph nodes and muscle ache.
- Lethargy and increased weakness in limbs. Dizziness, unsteady gait and collapse
- Intolerance to bright lights
- Migraine
- Partial face paralysis

Months after a tick bite from a paralysis tick, a tick induced mammalian meat allergy reaction may develop as an allergic reaction to red meat and gelatine.
If you have a tick and are experiencing a serious allergic reaction for the first time, seek urgent medical attention. Call 000 for an ambulance or go to the closest hospital emergency department.
If you have had similar symptoms in the past after being bitten by a tick and have a history of allergic reactions to tick bites, you should follow your allergy action plan and seek medical attention. If you are allergic to ticks, you should carry an adrenaline autoinjector (e.g. Anapen or EpiPen) for treating severe allergic reactions (anaphylaxis).
6. How do you remove a tick?

If you suffer from allergic reactions to ticks, only attempt to remove a tick when at a medical facility or a hospital Emergency Department.
For non- allergic individuals or for larval or nymphal stage ticks
- Before removal, spray the tick with an aerosol or cream insect repellent, containing pyrethrin. Apply at least twice with a 1min interval between applications.
- Use a FINE TIPPED forceps. Grasp the tick as close to the skin’s surface as possible. Pull upwards with steady pressure and avoid twisting, squeezing or sudden movement.
- When the tick is removed, clean the area with an antiseptic or soap and water. Tea tree oil is a good antiseptic that helps the body fight and relieve symptoms as well as acting as a repellent.
Some experts are now saying another possible method is to FREEZE the adult tick with a freezing pouch such as Elastoplast Cold Spray or Wart-Off Freeze, from a pharmacy (although currently these spray products are not intended to be used to kill ticks). These sprays contain either which freezes the tick and immediately killing it, so stopping it from injecting its saliva or regurgitating its contents into you. The tick will drop off in the next 24 hours and care must be taken not to compress or squeeze it.
Note that the Department of Health is not recommending this freezing method until further research becomes available. If you are unsure what to do, you can contact your doctor.
7. How do you Prevent Tick Bites?

The best way is to avoid tick infested areas, especially after rain. If this is not possible then:
- Apply insect repellent containing DEET- diethyl-meta-toluamide (e.g. Bushman, RID, Heavy Duty Aerogard or Tropical Aerogard) or picaridin (e.g. Aerogard) to the skin, clothes and hats.
- Treat clothing with permethrin (e.g. Equip Debugger). These are available from outdoor and camping shops. Permethrin wash kits for treating clothes can be obtained from outdoor recreational stores.
- Wear clothing that covers your body, a long-sleeved shirt tucked into your pants, long pants tucked into socks, wide brimmed hat.
- Wear light coloured clothing to make it easier to see ticks on clothes before they attach to the skin.
- When returning from outdoors, brush off your clothes to remove ticks before going inside. If you have visited a tick infested area clothing should be placed into a hot drier for 20min to kill any tick still on clothing.
- Shower and check for ticks of all sizes and stages especially to areas behind the ears and back of head or neck, especially on children.

If you live in a tick endemic area, make sure to keep some freeze spray and permethrin cream in your first-aid kit, so you are prepared should you get a tick or tick larvae.
8. How do you get a Tick Off your Dog?

If you find a tick on your dog it should be removed immediately. A vet can show you the best way, but it is important to keep your pet calm for tick paralysis cases.
- Wear disposable gloves. Have ready a small amount of alcohol into a zip lock bag or sealed container, to kill the tick once removed.
- Use tweezers or a purpose bought tick remover (a fork like device that slides either side of the tick).

- Aim to remove the tick by its head at the point of penetration into the pet’s skin. Do not squeeze the body.
- Twist and pull it out to help remove the mouth parts as well.
- Calmly do a quick search for any other ticks.
https://www.wikihow.com/video/9/9c/Remove%20a%20Tick%20Step%208.360p.mp4
If you do not have tweezers, dental floss can work just as well.
- Tie some thread around the mouthpart of the tick going as close to the skin as possible.
- Pull slowly, trying not to break the tick off so that the tick comes out completely.
If a tick is not removed properly, the main concern are the diseases that ticks can transmit. They can also cause a reaction that leads to a small abscess. In younger dogs a heavy infestation could lead to anaemia.
If the tick is left in the dog’s body, it will be expelled by itself. To avoid the chance of infection an antibiotic ointment can be applied.
9. Where can Ticks be Found in Australia?

Ticks occur in moist bushland, parks, and gardens especially on the Eastern most part of Australia. Tick populations tend to be higher in elevation, in long grassy or wooded areas where abundant native animals that they feed on live and roam including rabbits, deer, lizards, birds, mice, squirrels, and other rodents. They can sometimes be found in urban areas as well as on beaches in coastal areas.
The Gold Coast, Brisbane, Toowoomba and the Sunshine Coast areas all at risk of tick outbreaks. The Gold Coast is known as one of Australia’s hotspots for tick bites particularly joining Coffs Harbour and the NSW central and south coasts. Ticks thrive in warm humid environments and South East Queensland provides the perfect habitat for them.
10. What time of year are ticks around?

Ticks are active most of the year especially after rain and periods of high humidity. Their numbers are at their peak during the warmer months of Spring and Summer.
The tick has a distinct seasonality. The larval stage is the most active during Autumn months, the nymph during Winter and adult during Spring.

The ticks are not particularly mobile and rely on passing animals for their blood nourishment. The tick will crawl up stems of grasses or along branches and wait for a passing animal to latch onto, including humans! They generally do not climb higher than 50cm in their habitat and do not ‘drop’ out of trees. Once they land on a person or animal, they can walk up the body and attach to the head area.
Useful Links & Resources
● Ticks and tick bourne diseases protecting yourself (AABR)
● Tick Bite Prevention (Department of Health)
- Tick Bites (Health Direct)
https://www.healthdirect.gov.au/tick-bites
- Understanding and Preventing Tick Bites (Medline Plus)
https://magazine.medlineplus.gov/article/understanding-and-preventing-tick-bites
- Fact Sheet: Australian Paralysis Tick (Queensland Museum)
file:///C:/Users/hp/Downloads/fact-sheet-australian-paralysis-tick%20(2).pdf
- Lyme Disease (Department of Health)
https://www1.health.gov.au/internet/main/publishing.nsf/Content/ohp-lyme-disease.htm
- Lyme Disease Fact Sheet (NSW Health)
https://www.health.nsw.gov.au/Infectious/diseases/Pages/lyme-disease.aspx
