
Flesh eating bacteria that can cause serious wound infections, may sound like something out of a sci-fi movie!
This meat eating Buruli Ulcer is now on the rise in seaside towns in Eastern Australia.
Victoria seeing record numbers of the cases of this volcanic Buruli Ulcer this year, and with new outbreaks in NSW, researchers are investigating Possums as a culprit behind the spread along with mosquitoes.

1. What is a Buruli Ulcer?
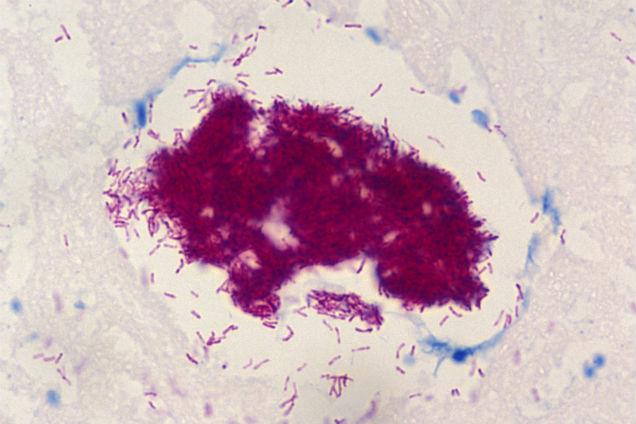
Buruli ulcer is an infection of the skin and soft tissue, caused by the bacterium Mycobacterium ulcerans.
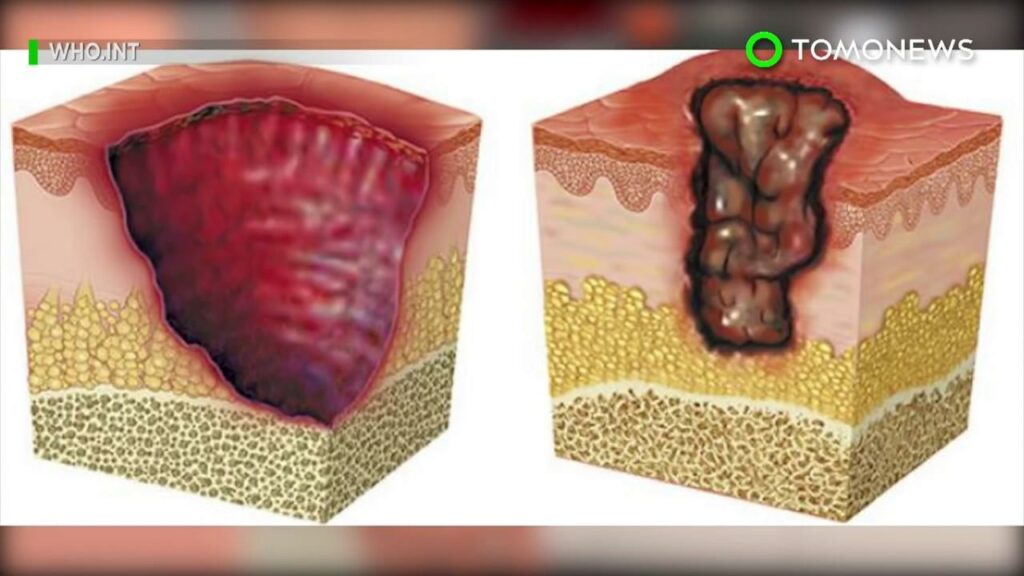
Toxins made by the bacteria attacks fat cells under the skin. This leads to localised redness and swelling or the formation of a nodule (lump) and then an ulcer. This can cause large open wounds and if untreated lead to permanent disfigurement.

The redness and swelling can be mistaken for an insect or spider bite. It can also sometimes be itchy. The symptoms of the Buruli ulcer can progress slowly over several weeks, but occasionally it can develop more rapidly. It may occur anywhere on the body but generally it is found on exposed areas of limbs such as forearms, elbow, back of calf, around the knee.

Although Buruli ulcer is not fatal, the infection can often leave people with noticeable cosmetic and severe tissue destruction. Sometimes functional damage to limbs that can last a lifetime.
2. How is the Buruli Ulcer spread?

How the Buruli Ulcer is transmitted was not fully understood until recently when the bacteria causing the ulcer was found in Possum excrement!!

Scientists have said that the ringtail and brushtail Possums are probably the key carrier. These wide eyed nocturnal also suffer from the disease and the Buruli bacteria are found in high quantities in their faeces.
As so much of the natural Possum habitat has been developed for housing in recent years, this is bringing Possums and humans closer together. Possums harbouring the bacteria in their gut pass it onto mosquitoes which infect humans. Humans who live in close quarters to possums are at an increased risk of the disease increasing.
Recently scientists are now investigating the hypothesis further by testing foxes and their faeces from a broad geographical area on the Bellarine Peninsula. A fox roams far and wide, so could possibly be involved in the transmission.
3. What conditions are needed for Buruli Ulcer transmissions?
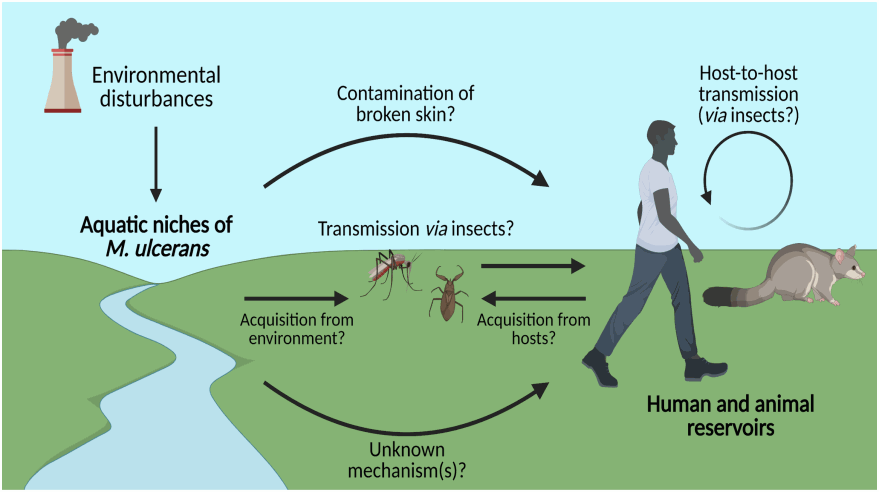
As human-to-human transmissions are extremely rare, and it is far more likely that the ulcer. This is because different elements are needed for transmission.
The different elements are needed are: –
- The introduction of bacteria into the environment by the native possums which have the disease.
- Hot and humid conditions for high densities of mosquitoes to flourish.
- High density of humans nearby which can be exposed to mosquito bites.
Given enough time and opportunity, the risk areas for Buruli ulcer could continue to grow across many more suburbs in Australia due to climate from the tropics in the north to the arid interior and temperate regions in the south.

4. What symptoms does a victim of Buruli ulcer have?

Symptoms of Buruli ulcer can include: –
- A painless swelling that looks like an insect bite on the upper or lower limb.

- The swelling grows bigger over days or weeks, often with no pain or fever.
- The swelling may form a crusty, non-healing scab.
- The scab then disintegrates into an ulcer within 4 weeks.
- The ulcer continues to enlarge.
- Unlike other ulcers, this ulcer is usually painless and there is generally no fever or other signs of infection.
- The infection may sometimes present with no ulceration but with localised pain. raised lumps, raised lumps, or thickened or raised flat areas of skin.
- Bone is occasionally affected causing deformities.

5. How is the Buruli Ulcer treated?

As the initial painless lump can be mistaken for an insect bite – early diagnosis is the key!
It can sometimes take between four to five months for and ulcer to develop after the victim is infected.
After a diagnosis the Buruli Ulcer is treated with a strong dose of two powerful antibiotics that need to be taken for often months.

An antibiotic called Rifampicin which is used in the treatment of extremely serious infections including leprosy and tuberculosis as well as moxifloxacin which is used to treat plague.
Depending on the seriousness of the ulcer, high doses of steroids and other interventions used to speed up the healing such as lymphoedema management. Surgery too is needed mainly including skin grafting to speed up the healing.
All patients have a good deal of suffering if the ulcer is not caught in time!
6. Where are outbreaks of the Buruli Ulcer occurring in Australia?

In Australia, the disease exists in Far North Queensland around the Mossman area, Northern Territory and in parts of Victoria. In Victoria, the disease is being identified in an increasing number of geographic areas, both coastal and non-coastal.
Recently NSW has had the first locally acquired case in the coastal town of Bateman’s Bay.
In recent years Victoria has been experiencing a record number of Buruli Ulcer cases. Cases of Buruli ulcer have been reported in southern areas of Victoria, the Bellarine, and Mornington Peninsulas, and in coastal regions of East Gippsland. In Melbourne, cases have also been reported in the south-eastern bayside areas and in, Moonee Ponds and Brunswick West and Essendon.
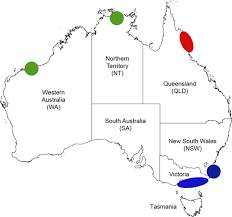
In NSW at least three cases of the flesh-eating ulcer have been reported but the good news is that these people who were affected from the NSW’s South coast are able to be treated and a warning has been issued for people to be wary of mosquitos!
However, with possums being mainly territorial animals there is still a mystery as to why the epidemic has been moving geographically!
7. What makes a person more at risk to develop a Buruli Ulcer?

A risk factor for contracting the disease is exposure to a Buruli-endemic area. The highest risk for infection is usually during the warmer months, but transmission can occur at any time of the year.
Even though the disease can occur at any age, a study has found that the Buruli ulcer notifications are highest in people aged 60 years and above in Victoria. Meanwhile another study has shown people with diabetes are two times more likely to be diagnosed with the ulcer. Tradies working outdoors, especially in contact with soil are also more likely to contract the disease.
Person to person transmission has so far not be detected but household members of people with Buruli Ulcer should keep a check on their own skin and any non-healing skin lesions or a persistent lump or swelling, especially if they have been exposed to the same environmental source.

8. What can you do to avoid a Buruli Ulcer?

Preventative methods include: –
- Reduce mosquito breeding sites around your home by reducing the areas where water can pool.
- Mosquito proof your home by securing insect screens.
- Wear loose fitting long pants and long-sleeved clothing when you’re outdoors, particularly if you’re working with the soil in the garden.
- Apply mosquito repellent to areas of skin that are exposed especially at dawn and dusk.
- Cover up any wounds, cuts, and abrasions with a dressing before encountering soil.
- Quickly wash any new scratches in soapy water and apply antiseptic cream on it, then a dressing.

9. What are the economic impacts of the Buruli Ulcer?
The Buruli Ulcer has serious health and economic consequences on any health authority.

The direct cost of the drugs and/or surgery, hospitalisation, testing, skilled nursing facilities, and rehabilitation has a heavy weighting.
Indirect costs of labour lost, effect on employers, with non-medical expenses of transport, accommodation and food for patients and caregivers easily mounts up.
The lost earnings from work impact any household. The treatment of steroids and the time needed to be on antibiotics leaves patients unwell tired, unmotivated, and even depressed. They are also open to oral and vaginal thrush and feeling sick with an upset stomach.
An early detection and antibiotic treatment are the cornerstones to economic control.

10. Possums be given a vaccine to control the Buruli Ulcer?

Controlling the disease in Possums would be an effective way of stopping both Possums and Humans getting Buruli ulcer. If the Possums are prevented from getting sick with the infection, then the chain of transmissions would be interrupted, and the disease could be eradicated.

Already, Oral bait BCG (Bacillus Calmette–Guérin) has been successful in controlling bovine tuberculosis in Possums. Mice that have been given BCG are immune to Buruli Ulcer.
This vaccine has been found to offer protection against the Buruli ulcer because tuberculosis is from the same bacterial family. Putting oral bait tuberculosis vaccines/BCG, out for the Possums to consume could offer limited protection against the Buruli Ulcer.

.
