
Australians have been warned to brace themselves for even more new and emerging diseases and viruses to jump from animals to humans.
Climate change is deemed the chief culprit and is aggravating more than half the know human diseases. This risk is a grave warning linking health impacts to global warming.
Diseases restricted to the tropics and other countries are creeping onto Australian shores with alarming acceleration. Diseases such as Monkeypox and COVID-19 are among the nearly 300 Australian diseases shown to be worsened by climate change.

1. What are the impacts of climate change on zoonotic diseases?
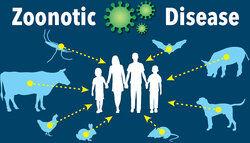
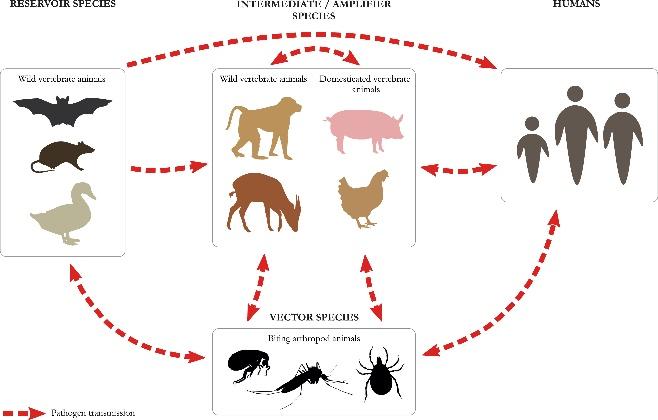
Zoonosis or zoonotic disease is a disease that has been passed into the human population from an animal source directly or through an intermediary species.
Zoonotic infections can be bacterial, viral, or parasitic in nature, with animal involvement playing a key role in maintaining such infections. Examples of zoonoses include Monkeypox, Covid-19, HIV-AIDS, Ebola, Lyme Disease and Malaria.
75% of all emerging infectious diseases in humans are zoonotic with a greater number of illnesses occurring at higher degrees of warming. If climate change continues humans must brace themselves for new emerging viruses and diseases to jump from animals to humans in the coming decades.
The increased use and exploitation of wildlife can bring humans in closer contact with wild animals, and so increasing the risk of zoonotic disease emergence. Warmer temperatures can increase the vector population size and distribution when infectious species are present in the environment.
2. What bat-borne diseases are aggravated by wildfires, drought, and deforestation?

Evidence shows that these events are contributing to occurrences of the Hendra virus. It causes severe or fatal infections in horses and humans. The virus’s natural host is fruit bats or ‘Flying Foxes’. A new type of Hendra virus is prevalent in Flying Foxes in South Australia. Victoria and Western Australia.

Hendra has never been reported to spread directly from Flying Foxes to humans as so far it has always been transmitted from infected horses to humans. Symptoms start with a fever, cough, sore throat, headache, and tiredness. Meningitis or Encephalitis (inflammation of the brain) can develop, causing headaches, high fever, and drowsiness, and sometimes convulsions and coma. Hendra virus infection can be fatal.
3. Which other bat-borne diseases are related to climate change in Australia?

Australian Bat Lyssavirus is shown to be worsened by climate change. It can be transferred to humans via a bite or a scratch from an infected bat. The Australian Bat Lyssavirus causes a serious illness which results in paralysis, convulsions, and delirium, and is fatal if not treated.
Natural reservoirs of the Menangle virus are in several species of fruit bats. It has been found to be a cause of serious illness in people who have caught it from an outbreak of the virus in pigs
4. Which serious diseases are aggravated by floods and increased rainfall?
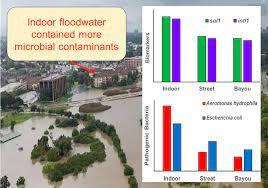
Bacteria which cause disease are displaced by heavy rain and floods. One organism which is associated with stagnant and swampy water is the Mycobacterium ulcertans once displaced from the soil leads to an increase in Buruli ulcers, a flesh-eating disease. The mycobacteria that cause tuberculosis and leprosy and many other environmental mycobacteria belong to this family.

Exposure to contaminated water can cause a potentially fatal bacterial infection called Melioidosis. The disease can lead to pneumonia, lesions in deep soft tissues and internal organs to soft tissue infection.
Leptospirosis is a bacterial disease in humans and animals. It is caused by Leptospira bacteria that are excreted in urine from infected animals including rats, mice, cattle, pigs, and dogs.
5. Which Insect borne diseases are climate sensitive?

Rainfall and temperature are factors that increase mosquito-borne diseases. Data has found that a combination of these excessive conditions in climate change has increased mosquito-borne disease prevalence, resulting in increased virus infections in humans.

Ross River virus disease is the most common and widespread mosquito-borne infection in Australia. Kangaroos and wallabies also carry the Ross River virus.
The appearance of Japanese encephalitis further south than its normal prevalence in Queensland is just the latest example of how global warming is contributing to the spread of the disease. The mosquitoes that carry it need pools of stagnant water, such as those created by the heavy downpours and the consequent floods.
Whilst the wetting of soil and increase surface water due to floods are factors there is a possibility that the loss of decontaminating ultraviolet light due to cloud cover and air pollution. This could cause further risk of diseases.

Climate change will also affect infectious disease occurrence. Several diseases well known to be climate-sensitive, such as Dengue fever, and Lyme disease, which is caused by ticks, are expected to worsen as climate change results in higher temperatures and more extreme weather events.
Other mosquito-borne infectious diseases that have been reported to be affected by global warming include the Barmah Forest virus, Kunjin virus infections and Murray Valley encephalitis.
6. Can climate change cause skin problems?

Many different skin diseases appear to be worsened by climate change. This includes inflammatory disorders such as eczema, and pemphigus an autoimmune blistering disease. Eczema can flare up for many reasons including air pollutants causing climate change. Chemical pollutants that are invisible can interrupt your skin’s natural protection system to break down your skin’s natural oils that would normally maintain the moisture in your skin, making your skin dry and irritable.

Ozone depletion results in people being exposed to higher levels of skin damage. Increasing temperature from climate change corresponds with an increase in UV radiation levels and so higher rates of skin cancer.

7. How does climate change affect airborne diseases?

Climate change affects air quality through several routes, including the production and allergenicity of allergens, and increases regional concentrations of ozone, fine particles, and dust.
The health effects of these disruptions in air quality include increased cardiovascular and respiratory disease. Australia is sensitive to such impacts because of its very high prevalence of allergic diseases such as Asthma and Hay Fever, and failure to tolerate to environmental allergens such as certain pollens and fungal spores leading to allergic inflammation.
8. Why are levels of Asthma so high in Australia?

The impacts of climate change on allergens and allergic diseases in Australia are a significant public health issue. The prevalence of Asthma and Hay fever (allergic rhinitis) in Australia is among the highest in the world!

The composition, abundance and exposure to airborne pollen or grass aeroallergens, for example, are strongly influenced by climate. The changes in the start and end date of the seasons increase exposure and the amounts of allergens in the air, making Australians highly vulnerable to the adverse impact of climate change on allergens and allergic diseases.

The world’s largest catastrophic epidemic thunderstorm asthma event occurred in Melbourne in 2016. The event was triggered by a sequence of environmental conditions resulting in extreme airborne grass pollen concentrations. This resulted in thousands of excess respiratory-related emergencies.
9. What are the projected changes in Australia’s climate that will affect health?

- More frequent and widespread extreme heat and heatwaves increase the risks of heat stress, heat stroke, dehydration, and mortality. Heatwaves contribute to acute cerebrovascular accidents and aggravate kidney, chronic respiratory and cardiac conditions, and psychiatric illness. Heatwave-related deaths will increase compared with current heat-related mortality.
- More frequent, prolonged, and widespread droughts, a significant cause of adverse mental health among rural Australians.

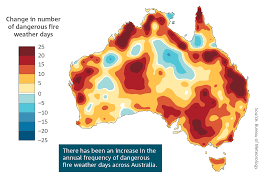
- More frequent, severe, and widespread bushfires, increasing risks of smoke inhalation, burns, heat stress, dehydration, trauma, and long-term mental health impacts.
- More extreme rainfall events, storm surges and flooding increase risks of injury, communicable disease transmission, distress, and acute and chronic anxiety disorders. With a rise in eco-anxiety due to constant media coverage, and concern about its impact.

10. Why is Australia most at risk and how can they keep disease at bay?
Australia has an already warm climate, making it more vulnerable than other countries to global warming.
Impacts of more frequent droughts and declining rainfall for areas like southwestern and south-eastern Australia would intensify with more global warming. Australians are already exposed to increased risk from drought, floods, heatwaves, fires, and invasive species.

Experts in Australia are increasingly recognising the need to monitor pest and disease outbreaks and improve responses. Early detection and early warning systems are critical tools to warn researchers, farmers, and policymakers of potential outbreaks.
Climate hazards have also made some aspects of pathogens more resilient and virulent. Higher levels of rainfall have allowed more mosquito-borne diseases to proliferate while stronger heatwaves have made diseases resistant to the body’s main protection systems.

Breeding pest and disease-resistant varieties of crops like wheat and maize is a solution. Beneficial insects can act as natural pest control for crops.
Rising temperatures and increased rainfall can promote an array of infectious diseases, from vector-borne diseases to parasitic diseases. As temperatures rise, larger quantities of spores are produced that can cause further infection and could potentially result in pathogenic changes through a faster rate of their evolution. Scientists need to understand how these changes bring people into closer contact with animals, pathogens, and arthropod vectors and alter the dynamics of diseases.
